Biologic Therapy for Asthma
For some patients with asthma avoidance of triggers and inhaled (and oral) medications are not enough to control their asthma. Recently, several new medications, known collectively as “biologics,” have been approved for the treatment of moderate-to-severe asthma. The term “biologic” is used for medications and other healthcare products that are made from living animals, plants, or cells, instead of through a chemical process. Biologics include a wide range of products, such as vaccines and blood products, as well as medications used to treat certain medical conditions (e.g., insulin for diabetes). Biologic therapies offer new ways of treatment because they target different molecules in the body that contribute to asthma. Biologic therapies can treat some types of severe asthma by helping to stop body processes that cause inflammation of the airways. This inflammation that may be caused by allergies or by high levels of a cell in the body called an eosinophil. Eosinophils are a type of white blood cell linked to inflammation. People with severe asthma sometimes have high levels of eosinophils in the blood.
If your provider is considering using a biologic to treat your asthma, the biologic would be added to the reliever and controller medications you are currently taking. Biologics do not replace these medications, although some people may find that they are able to reduce the dose of their controller medication after several doses of a biologic. Please note that you should only reduce the dose of your controller if your specialty provider tells you to do so.
Several options are available for biologic therapy in treating severe asthma with the so called allergic or eosinophilic phenotype. Severe allergic asthma where severe symptoms are triggered by allergies. This type of asthma mostly starts in childhood. Omalizumab is a biologic that targets severe allergic asthma, reducing the allergic response. Eosinophilic asthma where severe symptoms are triggered by higher levels of cells called eosinophils. This type of asthma is usually associated with adult-onset asthma. Mepolizumab, reslizumab and benralizumab are all biologics that target severe eosinophilic asthma, by reducing eosinophils. Severe asthma with type 2 inflammation where severe asthma symptoms are driven by both allergies and high levels of eosinophils. Dupilumab is a biologic targeting severe type 2 inflammatory asthma. It works by damping down the inflammatory response. The most recently approved biologic is a drug known as Tezepelumab. This targets an entirely different aspect of the asthma inflammatory cascade. Most of the therapies are given as an injection, either in the office, or using pre-filled syringes at home. Reslizumab is given through an intravenous infusion. Biologic treatment is given as an injection at your doctor’s office or special clinics, usually every 2 to 4 weeks, depending on the particular medication.
As with all medicines, biologic treatments can have risks and side effects. Some common side effects (affecting up to 1 in 10 people) include: headache, sinus pain, sore throat, soreness at the injection site (this should pass in a few days and may improve after you’ve had the injection a few times). Biologic treatments for asthma have an increased risk of a severe allergic reaction (anaphylaxis). The risk is rare (1 in 1000 or more) and more likely if you have a history of allergic reactions or anaphylaxis. This is not a complete list of the side effects that may happen with biologics; if your doctor is considering a biologic for you, please make sure to ask about the possible side effects that could happen with the specific medication you will be using.
There are currently no set recommendations on how long a patient should be on a biologic. Guidelines recommend trialing the medication for at least four months to see if it is helping improve your asthma. Your specialist may use tests to assess your status such as spirometry, FeNO, and blood tests. Whatever biologic you are prescribed, you will need to review your treatment regularly with your provider. Your doctor will work with you to decide how long to keep you on a biologic if your asthma is under good control. Contact your healthcare team if your asthma symptoms are not improving or are getting worse. Do not stop taking either your usual asthma medicines or your biologic treatment unless your doctor tells you to. If your treatment’s not working for you, or you’re getting difficult side effects, your specialist may stop treatment and look at other options.
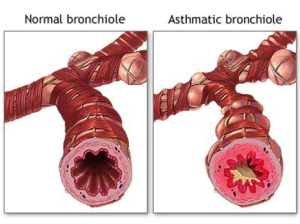 Asthma is a chronic disease that inflames and narrows the airways (the tubes that carry air into and out of your lungs). Asthma causes recurrent wheezing, chest tightness, shortness of breath, and cough. Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Inflammation in asthma makes the airways swollen and very sensitive. They tend to react strongly to certain substances that are breathed in. When the airways react, the muscles around them tighten. This causes the airways to narrow, and less air flows to your lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways may make more mucus than normal. Mucus can further narrow your airways.
Asthma is a chronic disease that inflames and narrows the airways (the tubes that carry air into and out of your lungs). Asthma causes recurrent wheezing, chest tightness, shortness of breath, and cough. Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Inflammation in asthma makes the airways swollen and very sensitive. They tend to react strongly to certain substances that are breathed in. When the airways react, the muscles around them tighten. This causes the airways to narrow, and less air flows to your lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways may make more mucus than normal. Mucus can further narrow your airways.