Although many people have bad reactions to certain foods, a true food allergy – a reaction triggered by the immune system – isn’t as common as you might think. However, the number of people who have a food allergy is growing. About 2 percent of adults and 6 percent of children have a true food allergy. Far more people have food intolerance, unpleasant symptoms triggered by food. Unlike a true food allergy though, a food intolerance doesn’t involve the immune system. A food allergy reaction occurs when your immune system overreacts to a food or a substance in a food, identifying it as a danger and triggering a protective response. Symptoms of a food allergy can range from mild to severe and typically appear within minutes to 2 hours after ingestion of a food to which he or she is allergic. Just because an initial reaction causes few problems doesn’t mean that all reactions will be similar; a food that triggered only mild symptoms on one occasion may cause more severe symptoms at another time. Symptoms of food allergy may include a tingling sensation in the mouth, swelling of the tongue and throat, difficulty breathing, hives, vomiting, abdominal cramps, diarrhea, low blood pressure, loss of consciousness, and even death. The most severe allergic reaction is called anaphylaxis – a life-threatening whole-body allergic reaction that can be fatal. It must be treated promptly. In some very rare cases, the reaction may be delayed by four to six hours or even longer. Delayed reactions are most typically seen in children who develop eczema as a symptom of food allergy and in people with a rare allergy to red meat caused by the bite of a lone star tick.
While any food can cause an adverse reaction, eight types of food account for about 90% of all reactions: Eggs, Milk and dairy, Peanuts, Tree nuts, Fish, Shellfish, Soy, Sesame. About 50% of children with allergies to milk, egg, soy, and wheat will outgrow their allergy by the age of 6. Those that don’t, and those still allergic by the age of 12 or so, have less than an 8% chance of outgrowing the allergy. Peanut and tree nut allergies are less likely to be outgrown, although evidence now shows that about 20% of those with peanut allergies and 9% of those with tree nut allergies will outgrow their allergies. However, one must never assume they have outgrown an allergy, and this should only be decided with the assistance of an allergy specialist.
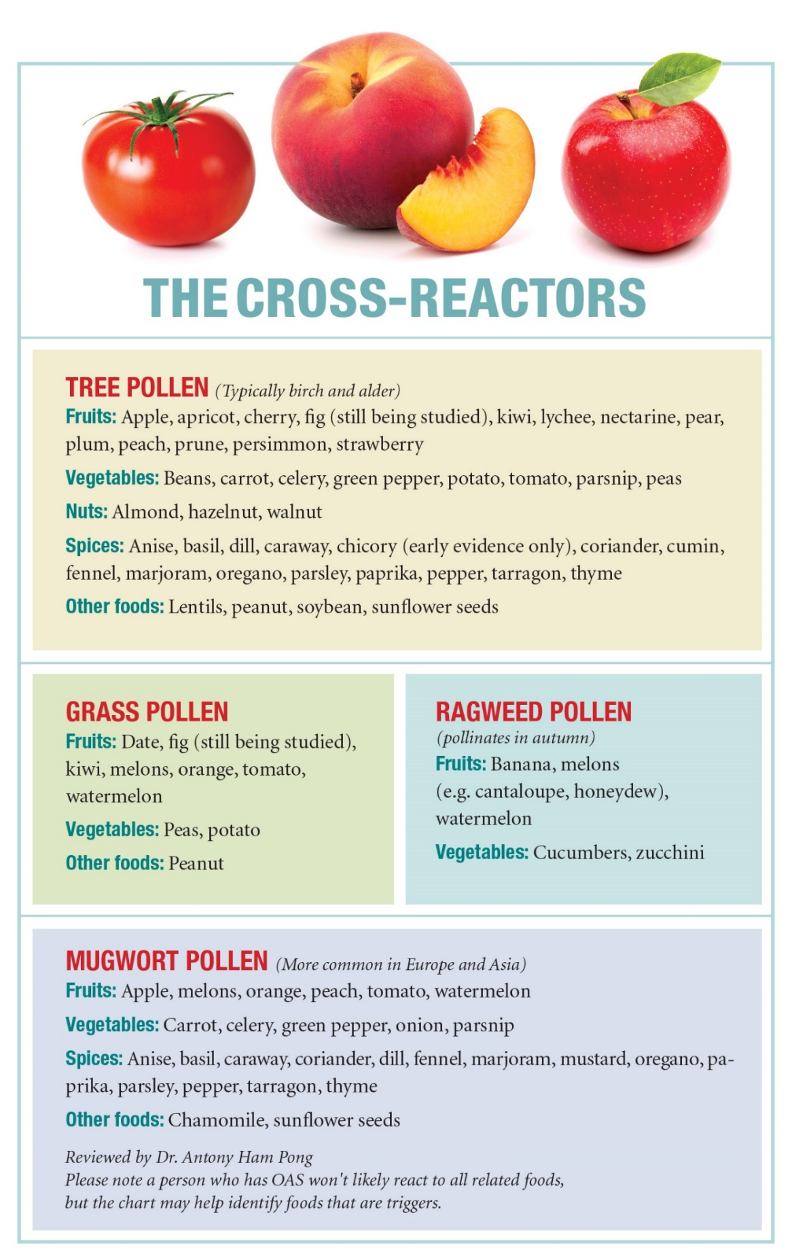
Not everyone who experiences symptoms after eating certain foods has a food allergy or needs to avoid that food entirely. Some people with seasonal allergy to pollens experience an itchy mouth and throat after eating a raw or uncooked fruit or vegetables. This may indicate a diagnosis of oral allergy (food-pollen) syndrome – a reaction to pollen, not to the food itself. The immune system recognizes the pollen and similar proteins in the food and directs an allergic response to it. The allergen is destroyed by heating the food, which can then be consumed with no problem. One can experience symptoms, primarily digestive, with a food intolerance. The most common example is lactose intolerance. Because a food intolerance may involve some of the same signs and symptoms as a food allergy does – such as nausea, vomiting, cramping and diarrhea – people often confuse the two. If you have a food in-tolerance, you may be able to eat small amounts of problem foods without a reaction. By contrast, if you have a true food allergy, even a tiny amount of food may trigger a severe allergic reaction.
Once a food allergy is diagnosed the most effective treatment is to avoid the food. People allergic to a specific food may also potentially have a reaction to related foods. For example, a person allergic to one tree nut may be cross-reactive to others. Those allergic to shrimp may react to crab and lobster. Learning about patterns of cross-reactivity and what must be avoided is one of the reasons why people with food allergies should receive care from an allergist. Determining if you are cross-reactive is not straightforward.
The primary way to manage a food allergy is to avoid consuming the food that causes you problems. Carefully check ingredient labels of food products and learn whether what you need to avoid is known by other names. The Food Allergy Labeling and Consumer Protection Act of 2004 (FALCPA) mandates that manufacturers of packaged foods produced in the United States identify, in simple, clear language, the presence of any of the eight most common food allergens in their products. The presence of the allergen must be stated even if it is only an incidental ingredient, as in an additive or flavoring. Be aware that FALCPA labeling requirements do not apply to items regulated by the U.S. Department of Agriculture (meat, poultry and certain egg products) and those regulated by the Alcohol and Tobacco Tax and Trade Bureau (distilled spirits, wine and beer). The law also does not apply to cosmetics, shampoos and other health and beauty aids, some of which may contain tree nut extracts or wheat proteins. Some goods also may be labeled with precautionary statements, such as “may contain,” “might contain,” “made on shared equipment,” “made in a shared facility” or some other indication of potential allergen contamination. There are no laws or regulations requiring those advisory warnings and no standards that define what they mean.
Symptoms caused by a food allergy can range from mild to life-threatening; the severity of each reaction is unpredictable. As noted, people who have previously experienced only mild symptoms may suddenly experience a life-threatening reaction. Therefore, allergists do not like to classify someone as “mildly” or “severely” food allergic – there is just no way to tell what may happen with the next reaction. Epinephrine is the first-line treatment for anaphylaxis. Once you have been diagnosed with a food allergy, your allergist should prescribe an epinephrine auto-injector and teach you how to use it. You should also be given a written treatment plan describing what medications you have been prescribed and when they should be used. Keep an eye on the expiration date of your auto-injector. Anyone with a food allergy should always have the auto-injector close at hand. Having two doses available is important as the severe reaction can recur in about 20% of individuals. Use epinephrine immediately if you experience severe symptoms such as shortness of breath, repetitive coughing, weak pulse, hives, tightness in your throat, trouble breathing or swallowing vomiting, diarrhea or abdominal pain. You should call for an ambulance to be taken to the emergency room. Inform the dispatcher that epinephrine was administered and more may be needed. If you are uncertain whether a reaction warrants epinephrine, use it right away; the benefits of epinephrine far outweigh the risk that a dose may not have been necessary.
Common side effects of epinephrine may include anxiety, restlessness, dizziness and shakiness. In very rare instances, the medication can lead to abnormal heart rate or rhythm, heart attack, an increase in blood pressure and fluid buildup in the lungs. If you have certain pre-existing conditions, such as heart disease or diabetes, you may be at a higher risk for adverse effects from epinephrine. Nevertheless, epinephrine is considered very safe and is the most effective medicine to treat severe allergic reactions. Other medications may be prescribed to treat symptoms of a food allergy, but it is important to note that there is no substitute for epinephrine: It is the only medication that can reverse the life-threatening symptoms of anaphylaxis.