Asthma
What is Asthma
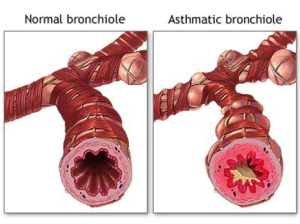 Asthma is a chronic disease that inflames and narrows the airways (the tubes that carry air into and out of your lungs). Asthma causes recurrent wheezing, chest tightness, shortness of breath, and cough. Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Inflammation in asthma makes the airways swollen and very sensitive. They tend to react strongly to certain substances that are breathed in. When the airways react, the muscles around them tighten. This causes the airways to narrow, and less air flows to your lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways may make more mucus than normal. Mucus can further narrow your airways.
Asthma is a chronic disease that inflames and narrows the airways (the tubes that carry air into and out of your lungs). Asthma causes recurrent wheezing, chest tightness, shortness of breath, and cough. Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Inflammation in asthma makes the airways swollen and very sensitive. They tend to react strongly to certain substances that are breathed in. When the airways react, the muscles around them tighten. This causes the airways to narrow, and less air flows to your lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways may make more mucus than normal. Mucus can further narrow your airways.
Sometimes symptoms are mild and go away on their own or after minimal treatment with an asthma medicine. At other times, symptoms continue to get worse. When symptoms get more intense and/or additional symptoms appear, this is an asthma attack. It’s important to treat symptoms when you first notice them. This will help prevent the symptoms from worsening and causing a severe asthma attack. Severe asthma attacks may require emergency care, and they can cause death. Asthma cannot be cured. Even when you feel fine, you still have the disease and it can flare up at any time. With proper treatment, most people who have asthma can expect to have few, if any, symptoms either during the day or at night.
How is Asthma Diagnosed?
Asthma is often diagnosed clinically – a diagnosis based on signs, symptoms and examination. The diagnosis however, even if made by a physician, may not be correct. Asthma is more accurately diagnosed with a breathing test, called a PFT – pulmonary function tests. The most common PFT is called spirometry. Your provider though may want you to have a more specific test known as a methacholine challenge test. Follow the links for more information.
https://www.thoracic.org/patients/patient-resources/resources/pulmonary-function-tests.pdf
https://www.thoracic.org/patients/patient-resources/resources/lung-function-studies-methacholine.pdf
How is Asthma Treated?
Once you are diagnosed with asthma, it is very important that you work closely with your provider to control your asthma. You and your provider can develop an Action Plan that you will follow to treat your symptoms and improve your breathing. Your Action Plan will include when to take your medications, what you can do in your daily life to avoid triggers, and how to monitor your breathing.
One of the central tenants of asthma care is known as Lifestyle Management. This begins with learning what specific “triggers” may be causing your asthma symptoms. Keep a journal to track your day-to-day activities along with any symptoms that you may be having during the day or at night. Once you know what may be causing your asthma, you can then try to stay away from those triggers. Asthma Triggers include:
- Respiratory tract infections
- Allergens (e.g., dust mites, cats & dogs, molds)
- Chronic sinusitis
- Exercise
- Cigarette smoke (1st and 2nd hand)
- Vaping and hookah
- Gastroesophageal reflux disease
- Medications (e.g., Beta-blockers, Aspirin)
Stay healthy: Eat nutritious foods and get regular exercise. Avoid people who smoke and those that may have an infection, especially a cold or the flu. Cope with stress: Learn new ways to cope with stress. Coping with stress can help prevent and control your asthma.
Medications will be prescribed that keep your airways open and reduce swelling, so air can move in and out of your lungs more easily. First line therapy is with a short-acting bronchodilator, most commonly albuterol or levalbuterol. This is known as ‘reliever’ or ‘rescue’ therapy and is used as needed for symptom relief. These medications relax the muscles that have constricted around the airway. Use of an inhaler may not be as easy as it looks. Make sure you review proper technique with your provider. You can follow the link below for additional tips on their proper use.
https://www.thoracic.org/patients/patient-resources/resources/metered-dose-inhaler-mdi.pdf
If your asthma symptoms are more persistent – for example, you require use of your albuterol more than twice per week, or you wake because of your asthma more than twice a month, your provider will start you on what is known as ‘controller’ or maintenance therapy. Unlike the short acting bronchodilator, these medications must be taken every day. The mainstay of therapy is the inhaled corticosteroid (ICS). The medications provide anti-inflammatory therapy to the airways thereby reducing inflammation, mucous production and airway responsiveness (the ability for the airway to constrict too easily). The ICS may be combined with a long-acting bronchodilator (LABA). These are used once or twice per day. The inhalers come in the traditional form of a metered dose inhaler (MDI) or what is termed a dry-powder inhaler (DPI). The medications are identical. Patient preference should guide the choice. Other add on therapies are available if needed to achieve control. Some of these may be in pill form including leukotriene modifying drugs (montelukast, zafirlukast) and theophylline. These drugs are not usually as effective as corticosteroids and long-acting bronchodilators. A new class of specialized asthma therapies are now available for individuals with difficult to control (moderately severe asthma). These are known as biologic therapies. Your provider may order additional blood work or allergy testing to see if you woud be a candidate for these.
What else?
It is important that you work with your provider to find a treatment plan that works for you and controls your asthma. Peak flow monitoring may also be recommended. Measuring your peak flow (a form of a pulmonary function test) by blowing into a peak flow meter can provide a measure of your asthma control. Sometimes your peak flow reading can make you aware that your asthma is worsening before you have symptoms. The goal of peak flow monitoring is to help guide you to prevent an asthma attack. Always carry your rescue inhaler with you. Take your asthma medication exactly as your health care provider has advised. Get a yearly flu shot and a vaccine for pneumonia. Keep your regularly scheduled visits with your provider so that your asthma can be monitored and treated before it gets out of control. Be sure to know how to contact your health care provider and know what to do in case of an emergency. If your asthma is not getting better after you start treatment, you might benefit from seeing an asthma specialist.
Take the Asthma Control Test™ – https://www.asthma.com/understanding-asthma/severe-asthma/asthma-control-test/
Other Asthma Resources